Expecting mothers often wonder what they should eat to support their health and their baby’s development. A well-balanced diet plays a crucial role in ensuring both mom and baby thrive. In 2025, updated guidelines from the USDA and WHO highlight the importance of specific nutrients for women during this special time.
These essential nutrients not only help prevent birth defects but also support fetal growth and development. From folate to iron, each nutrient has a unique role in promoting lifelong health for both mother and child. Staying informed about these recommendations can make a significant difference.
Later sections will also explore weight management and calorie needs, ensuring you have a comprehensive understanding of what to focus on. Let’s dive into the key nutrients that should be part of every expecting mother’s diet.
Key Takeaways
- 2025 dietary guidelines emphasize specific nutrients for expecting mothers.
- Proper prenatal nutrition impacts both maternal and fetal health.
- Key nutrients help prevent birth defects and support development.
- Updated USDA and WHO recommendations provide essential insights.
- Weight management and calorie needs are also critical for a healthy pregnancy.
Introduction to Nutrition During Pregnancy
Pregnancy brings unique dietary needs that support both mom and baby. A balanced diet is essential to meet these demands. Women expecting a child often require 30-50% more nutrients than usual. This ensures the growing baby gets everything needed for healthy development.
The placenta plays a key role in transferring nutrients from mom to fetus. It acts as a bridge, delivering vitamins, minerals, and other essentials. Without proper intake, this process can be compromised, affecting both maternal and fetal health.
In 2025, dietary guidelines emphasize food quality over quantity. Instead of focusing on calorie counts, experts recommend choosing nutrient-dense foods. These are packed with vitamins and minerals, providing more benefits per bite.
Nutrient density is a critical concept for expecting moms. Foods like leafy greens, lean proteins, and whole grains are excellent choices. They offer high levels of essential nutrients without excess calories.
Both undernutrition and overnutrition pose risks. Too few nutrients can lead to deficiencies, while excessive intake may cause complications. Striking the right balance is key to a healthy pregnancy.
| Nutrient | Role | Food Sources |
|---|---|---|
| Folic Acid | Prevents birth defects | Spinach, citrus fruits |
| Iron | Supports oxygen transport | Red meat, beans |
| Calcium | Builds bones and teeth | Dairy, fortified plant milk |
| Vitamin D | Enhances calcium absorption | Sunlight, fatty fish |
The Role of Folic Acid in Pregnancy
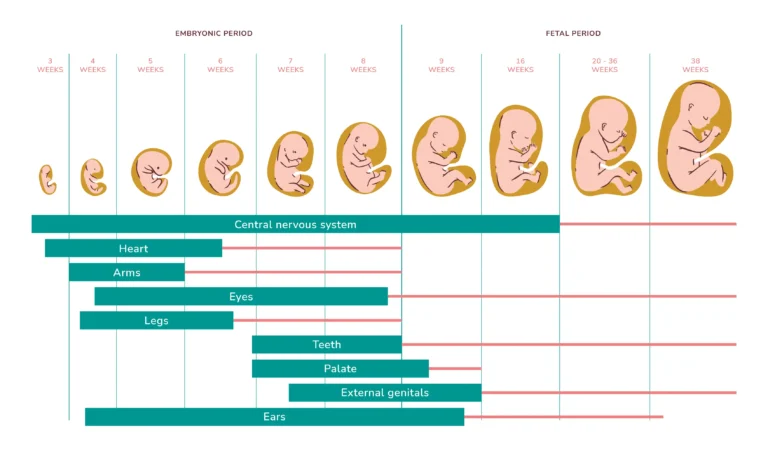
Folic acid is a key nutrient that plays a vital role in the early stages of fetal development. It’s especially important in the first 28 days when the neural tube forms. This structure eventually becomes the baby’s brain and spinal cord. Without enough folic acid, the risk of birth defects like spina bifida increases significantly.
Natural sources of folic acid include leafy greens, citrus fruits, and fortified cereals. However, meeting the daily requirement through diet alone can be challenging. That’s why many healthcare providers recommend supplements to ensure adequate intake.
Why Folic Acid is Crucial
Folic acid helps the body produce and maintain new cells, which is critical during rapid fetal growth. It also supports the development of the baby’s neural tube, which closes by the fourth week of pregnancy. A deficiency can lead to serious complications, including anemia and preterm birth.
Recommended Daily Intake
In 2025, updated guidelines recommend 400 mcg of folic acid daily before conception and 600 mcg during pregnancy. These amounts help reduce the risk of neural tube defects and support overall maternal health. If you’re planning to conceive or are already expecting, consult your doctor about the right supplements for you.
- Neural tube formation occurs in the first 28 days.
- Leafy greens and fortified cereals are excellent sources.
- Supplements are often necessary to meet daily needs.
- Deficiency can lead to anemia and preterm birth.
Iron: Supporting Baby’s Growth and Development
Iron is a powerhouse nutrient that plays a critical role in ensuring a healthy journey for both mom and baby. It’s essential for producing hemoglobin, a protein in blood that carries oxygen to tissues and organs. During this time, a woman’s blood volume increases by up to 50%, making iron even more vital.
Iron also supports fetal brain development, helping your baby grow strong and healthy. Without enough iron, both mom and baby can face challenges like fatigue, anemia, and even low birth weight. Ensuring adequate intake is key to a smooth and healthy experience.
The Importance of Iron
Iron’s primary role is to support oxygen transport throughout the body. This is especially important as the body works harder to support both mom and baby. A deficiency can lead to serious complications, including reduced energy levels and impaired fetal growth.
“Iron is not just a nutrient; it’s a lifeline for both mother and baby.”
To maximize iron absorption, pair iron-rich foods with sources of vitamin C, like oranges or bell peppers. This combination helps the body absorb iron more efficiently, ensuring you get the most out of your diet.
Iron-Rich Foods
Including iron-rich foods in your meals is a simple way to meet your daily needs. Here are some top sources:
- Lean meats like beef and chicken
- Legumes such as lentils and beans
- Leafy greens like spinach and kale
If you’re taking iron supplements, be aware they can sometimes cause constipation. Drinking plenty of water and eating fiber-rich foods can help alleviate this issue.
| Food | Iron Content (per serving) |
|---|---|
| Spinach | 6.4 mg |
| Lentils | 6.6 mg |
| Beef | 2.6 mg |
By prioritizing iron-rich foods and pairing them with vitamin C, you can ensure you’re meeting your daily needs and supporting your baby’s growth and development.
Calcium: Building Strong Bones and Teeth
Calcium is a cornerstone for building a strong foundation for both mom and baby. This essential mineral supports fetal skeletal development, ensuring the baby’s bones and teeth form properly. It also plays a critical role in maintaining maternal bone health and muscle function.
Why Calcium is Essential
During pregnancy, the baby relies on calcium from the mother’s diet to develop its skeleton. This process begins as early as the first trimester and continues throughout. Adequate calcium intake can also reduce the risk of preeclampsia by 25%, making it a vital nutrient for both mom and baby.
Calcium works in synergy with vitamin D to enhance absorption. Without enough vitamin D, the body struggles to utilize calcium effectively. This partnership ensures that both nutrients contribute to optimal health.
How Much Calcium You Need
Adults need about 1,000 mg of calcium daily, while teens require 1,300 mg. Meeting these needs can be achieved through a combination of diet and supplements. Dairy products like milk, cheese, and yogurt are excellent sources. For those with lactose intolerance, fortified plant-based alternatives like almond or soy milk are great options.
- Fetal skeletal development begins in the first trimester.
- Dairy and non-dairy sources both provide essential calcium.
- Vitamin D enhances calcium absorption for better results.
- Lactose-free options ensure everyone can meet their needs.
- Calcium supports muscle function and bone health.
“Calcium isn’t just about bones; it’s about building a healthy future for both mother and baby.”
Vitamin D: Enhancing Calcium Absorption
Vitamin D is a crucial nutrient that works hand-in-hand with calcium to support maternal and fetal health. It helps the body absorb calcium more efficiently, ensuring strong bones and teeth for both mom and baby. Without enough vitamin D, calcium absorption is compromised, which can lead to complications like rickets in infants or osteoporosis in mothers.
The Role of Vitamin D
Vitamin D comes in two forms: D2 and D3. D3, found in animal products and sunlight, is more effective at raising blood levels of the vitamin. It supports immune function, reduces inflammation, and plays a key role in fetal skeletal development. A deficiency can increase the risk of gestational diabetes and preeclampsia.
According to NHANES data, 40% of expecting mothers are deficient in vitamin D. This highlights the importance of meeting the daily requirement of 600 IU. Testing your levels is a simple way to ensure you’re on track.
Sources of Vitamin D
Getting enough vitamin D can be achieved through a combination of diet, supplements, and safe sun exposure. Fatty fish like salmon and mackerel are excellent natural sources. Fortified foods, such as milk and cereals, also provide a significant boost.
Spending time in the sunlight is another effective way to increase vitamin D levels. Aim for 10-15 minutes of midday sun exposure a few times a week. However, always use sunscreen to protect your skin from harmful UV rays.
- Vitamin D3 is more effective than D2 for raising blood levels.
- Fortified foods like milk and cereals are great dietary sources.
- Safe sun exposure can help maintain adequate levels.
- Deficiency increases risks like gestational diabetes and rickets.
- Testing is recommended to monitor vitamin D levels.
“Vitamin D isn’t just about bones; it’s about building a healthy future for both mother and baby.”
Protein: Supporting Tissue Growth
Protein plays a pivotal role in ensuring both maternal and fetal health. It’s essential for building new tissues, supporting placental development, and aiding fetal cell growth. During this time, the body’s need for protein increases by about 25 grams per day to meet these demands.
Protein is made up of amino acids, which are the building blocks of life. These compounds are critical for creating new cells and repairing tissues. Without enough protein, both mom and baby may face challenges like slowed growth or developmental issues.
Why Protein is Important
Protein supports the growth of the placenta, which nourishes the baby throughout the journey. It also helps develop the baby’s muscles, organs, and tissues. As the body works harder to support both mom and baby, adequate protein intake becomes even more crucial.
Different trimesters have varying protein needs. In the first trimester, the focus is on placental development, while later trimesters emphasize fetal growth. Meeting these needs ensures a smooth and healthy experience for both.
Healthy Protein Sources
Animal-based proteins like eggs and poultry are excellent sources of complete proteins, meaning they contain all essential amino acids. For vegetarians and vegans, plant-based options like quinoa, lentils, and nuts can provide the necessary nutrients.
- Greek yogurt: High in protein and calcium.
- Quinoa: A complete plant-based protein.
- Chicken breast: Lean and packed with protein.
- Almonds: A great source of protein and healthy fats.
“Protein isn’t just about muscle; it’s about building a healthy future for both mother and baby.”
By incorporating a variety of protein sources into your diet, you can ensure you’re meeting your daily needs and supporting your baby’s growth and development.
Omega-3 Fatty Acids: Boosting Brain Development
Omega-3 fatty acids are essential for supporting both maternal health and fetal brain development. These healthy fats, particularly DHA and EPA, play a critical role in ensuring your baby’s cognitive growth and overall well-being. Research shows that DHA alone contributes to 70% of fetal brain development, making it a must-have nutrient.
The Benefits of Omega-3s
DHA and EPA are the two primary types of omega-3s. DHA is crucial for brain and eye development, while EPA supports heart health and reduces inflammation. Together, they help build a strong foundation for your baby’s future.
Studies have linked adequate omega-3 intake to improved cognitive outcomes in children. These benefits extend beyond pregnancy, supporting long-term brain health and function.
Best Sources of Omega-3s
Fatty fish like salmon, sardines, and mackerel are excellent sources of omega-3s. However, it’s important to limit high-mercury options like albacore tuna to 6 ounces per week. For those who prefer plant-based options, algae-based supplements are a great alternative.
Here are some safe and effective ways to include omega-3s in your diet:
- Salmon: Rich in DHA and EPA.
- Sardines: A low-mercury, nutrient-dense choice.
- Algae oil: A vegan-friendly source of DHA.
“Omega-3s aren’t just good for the brain; they’re essential for building a healthy future for both mother and baby.”
By incorporating these sources into your meals, you can ensure you’re meeting your omega-3 needs and supporting your baby’s development.
Fluids: Staying Hydrated During Pregnancy
Staying hydrated is one of the simplest yet most impactful ways to support a healthy journey for both mom and baby. During this time, a woman’s blood volume increases by up to 50%, making proper fluid intake essential. Adequate hydration helps maintain amniotic fluid levels, which cushion and protect the baby.

Dehydration can lead to serious complications, including preterm labor. That’s why it’s crucial to drink at least 10 cups of water daily. Paying attention to your body’s signals, like the color of your urine, can help you stay on track. Pale yellow is a good indicator of proper hydration.
The Importance of Hydration
Hydration supports critical functions like nutrient transport and waste removal. It also helps regulate body temperature, which is especially important during this time. Electrolytes, such as sodium and potassium, play a key role in maintaining fluid balance. Including electrolyte-rich foods or drinks can help keep levels stable.
Herbal teas can be a soothing option, but it’s important to choose caffeine-free varieties and consult your doctor. Some herbs may not be safe for expecting mothers. Always prioritize water as your main source of hydration.
How Much Water You Need
On average, women need about 10 cups of fluids daily. This amount may vary based on activity level, climate, and individual needs. Morning sickness can make it challenging to stay hydrated, so sipping small amounts throughout the day is a helpful strategy.
- Amniotic fluid levels depend on proper hydration.
- Pale yellow urine indicates good hydration.
- Electrolytes help maintain fluid balance.
- Herbal teas should be caffeine-free and doctor-approved.
- Small, frequent sips can help with morning sickness.
“Hydration isn’t just about drinking water; it’s about supporting a healthy future for both mother and baby.”
How Much Weight Should You Gain During Pregnancy?
Understanding the right amount of weight to gain is a common concern for many women. The ideal range depends on your pre-pregnancy BMI, ensuring both mom and baby stay healthy.
For those with a normal BMI (18.5–24.9), the recommended gain is 25–35 pounds. If your BMI falls into the obese category (30+), the range narrows to 11–20 pounds. These guidelines help reduce risks like gestational diabetes or high birth weight.
Most of the weight is gained in the third trimester as the baby grows rapidly. However, the first and second trimesters also play a role in building the placenta and increasing blood volume.
Excessive gain can lead to complications like preeclampsia or a difficult delivery. On the other hand, gaining too little may result in low birth weight or preterm birth. Striking the right balance is key.
- Normal BMI: 25–35 pounds
- Overweight BMI: 15–25 pounds
- Obese BMI: 11–20 pounds
- Underweight BMI: 28–40 pounds
Tracking your progress can help you stay on target. Apps and tools like MyFitnessPal or a simple journal make it easy to monitor your weight and ensure a healthy journey.
“Healthy weight gain isn’t just about numbers; it’s about supporting a healthy future for both mother and baby.”
Do You Need Extra Calories During Pregnancy?
Calorie needs shift as your body supports both you and your growing baby. While the idea of “eating for two” is a common myth, the reality is more nuanced. Your body’s energy demands increase, but the focus should be on nutrient-dense foods rather than simply consuming more.
In the second trimester, you’ll need about 340 extra calories daily. By the third trimester, this increases to 450. These numbers account for changes in your basal metabolic rate (BMR), which rises to support fetal growth and maternal health.
Not all calories are created equal. Choosing whole foods like fruits, vegetables, lean proteins, and whole grains ensures you’re meeting your needs without empty calories. Snacks like Greek yogurt with berries or a handful of nuts are excellent options.
For those with gestational diabetes, managing calorie intake becomes even more critical. Focus on balanced meals with complex carbs, lean proteins, and healthy fats. This approach helps stabilize blood sugar levels while supporting your baby’s development.
“Quality over quantity is the key to meeting your calorie needs during this special time.”
By understanding your body’s changing needs, you can make informed choices that benefit both you and your baby. Prioritize nutrient-dense foods and consult your doctor for personalized advice.
Foods to Avoid During Pregnancy
Certain foods can pose risks to both mom and baby, making it essential to know what to avoid. While many items are safe and nutritious, others carry hidden dangers that could impact health. Staying informed helps ensure a smoother and safer journey.
High-Mercury Fish
Some types of fish contain high levels of mercury, which can harm fetal brain development. Avoid shark, swordfish, and king mackerel. Instead, opt for safer options like salmon or sardines, which are rich in omega-3s without the risks.
Unpasteurized Foods
Unpasteurized dairy products and juices can harbor harmful bacteria like listeria. Soft cheeses such as brie and feta should be avoided unless labeled pasteurized. Always check labels to ensure safety.
Here are some additional tips to keep in mind:
- Avoid raw or undercooked meat, eggs, and sprouts to prevent foodborne illnesses.
- Cook all meat to safe internal temperatures to kill harmful bacteria.
- Store perishable foods properly to maintain freshness and safety.
- When dining out, ask about ingredient preparation to avoid risks.
- While traveling, stick to bottled water and avoid street foods of unknown origin.
“Being cautious about what you eat isn’t just about avoiding risks; it’s about ensuring a healthy future for both mother and baby.”
Healthy Eating Tips for Pregnant Women
Eating well is one of the best ways to support your health and your baby’s growth. A balanced diet rich in fruits, vegetables, and whole grains can make a big difference. The WHO recommends at least five portions of fruits and veggies daily, so aim for a colorful plate at every meal.
Meal planning is a great strategy to stay on track. Prepare weekly menus that include a mix of lean proteins, healthy fats, and complex carbs. This helps you avoid last-minute unhealthy choices and ensures you’re meeting your nutritional needs.
Snacking smart is another key tip. Swap sugary treats for nutrient-dense options like nuts, yogurt, or fresh fruit. These choices keep your energy levels steady and provide essential vitamins and minerals.
Cravings are common, but managing them wisely is important. If you’re craving something sweet, try a small piece of dark chocolate or a fruit smoothie. For salty cravings, opt for air-popped popcorn or roasted chickpeas.
Eating out doesn’t have to derail your diet. Look for grilled or baked options, and ask for dressings or sauces on the side. Many restaurants are happy to accommodate special requests, so don’t hesitate to ask.
Finally, eating healthy doesn’t have to break the bank. Buy seasonal produce, cook at home, and use leftovers creatively. These budget-friendly tips ensure you can nourish yourself and your baby without overspending.
“A colorful plate isn’t just visually appealing; it’s a simple way to ensure you’re getting a variety of nutrients.”
The Importance of Prenatal Supplements
Ensuring proper nutrient intake is vital for both mom and baby, and supplements can play a key role. Studies show that 90% of women need additional support to meet their daily requirements. Choosing USP-verified brands ensures quality and safety.
Timing matters when taking supplements. Pairing them with meals can improve absorption and reduce nausea. If morning sickness is an issue, try smaller doses throughout the day or opt for chewable options.
For those following a plant-based diet, vegan formulations are available. These provide essential vitamins like folic acid and iron without animal-derived ingredients. Always check labels to ensure they meet your dietary preferences.
It’s also important to consider potential drug interactions. Consult your healthcare provider before starting any new supplements, especially if you’re on medication. This helps avoid complications and ensures compatibility.
Postpartum continuation of supplements can support recovery and breastfeeding. Many women find that maintaining their regimen helps replenish nutrient stores and boosts energy levels during this demanding time.
“Supplements aren’t just a convenience; they’re a lifeline for meeting the unique needs of this special journey.”
- Take supplements with meals for better absorption.
- Choose vegan options if following a plant-based diet.
- Consult your doctor to avoid drug interactions.
- Continue taking supplements postpartum for recovery.
- Opt for USP-verified brands for quality assurance.
By incorporating supplements into your routine, you can ensure you’re meeting your nutritional needs and supporting your baby’s development. Always prioritize safety and consult your healthcare provider for personalized advice.
Common Nutritional Challenges During Pregnancy
Navigating dietary changes can be challenging for many women during this special time. From morning sickness to unusual cravings, these hurdles are common but manageable. Understanding how to address them can make a big difference in your overall well-being.
Morning sickness affects up to 85% of women, often making it hard to stick to a balanced diet. Small, frequent meals and ginger-based remedies can help ease nausea. Staying hydrated is also key, as dehydration can worsen symptoms.
Pica cravings, which involve non-food items like ice or clay, occur in about 60% of women. These cravings may signal nutrient deficiencies, such as iron or zinc. Consulting your doctor can help identify and address the root cause.
Food aversions are another common issue. Strong smells or textures may turn you off from certain foods. Experimenting with alternatives or preparing meals in advance can help you maintain a nutritious intake.
GERD, or acid reflux, is a frequent complaint. Eating smaller portions, avoiding spicy foods, and not lying down immediately after meals can provide relief. Constipation is also common, but increasing fiber and water intake can help.
Anemia prevention is crucial, as iron needs rise significantly. Including iron-rich foods like spinach, lentils, and lean meats in your diet can help. Pairing them with vitamin C sources enhances absorption.
Gestational diabetes requires careful management. Focus on balanced meals with complex carbs, lean proteins, and healthy fats. Regular monitoring and exercise can also help stabilize blood sugar levels.
“Facing these challenges head-on isn’t just about feeling better; it’s about ensuring a healthy future for both mother and baby.”
By addressing these common issues, you can create a smoother and healthier journey for yourself and your baby. Always consult your healthcare provider for personalized advice.
Planning Your Pregnancy Diet
Crafting a balanced diet tailored to your needs is essential for a healthy journey. The USDA MyPlate guidelines offer a great starting point, but modifications can help you meet your unique requirements. Focus on a 40-30-30 macronutrient ratio—40% carbs, 30% protein, and 30% fats—to ensure you’re getting the right mix of energy and building blocks.
Creating a trimester-specific plan ensures your diet evolves with your baby’s growth. In the first trimester, prioritize foods rich in folate and iron. By the second trimester, increase your calorie intake with nutrient-dense options. In the final trimester, focus on foods that support rapid fetal development and prepare your body for delivery.
Cultural adaptations can make your diet more enjoyable and sustainable. Incorporate traditional foods that align with your nutritional needs. For example, swap white rice for quinoa or add lentils to soups for an iron boost. This approach keeps your meals flavorful while meeting your requirements.
Tracking your intake through food journaling helps you stay on top of your nutrients. Note what you eat, how you feel, and any cravings or aversions. This practice can reveal patterns and help you adjust your diet for better results.
Collaborating with a nutritionist ensures your meals are optimized for your health and your baby’s development. They can provide personalized advice, address deficiencies, and help you navigate challenges like morning sickness or food aversions.
Finally, plan for the postpartum transition. Your body will need time to recover, and your diet should support healing and breastfeeding. Focus on foods rich in iron, calcium, and omega-3s to replenish your nutrient stores and maintain energy levels.
“A well-planned diet isn’t just about eating right; it’s about creating a foundation for lifelong health for both you and your baby.”
Conclusion: Prioritizing Nutrition During Pregnancy
Taking care of your diet now sets the stage for a healthier future for you and your baby. From folate to omega-3s, each nutrient plays a vital role in supporting growth and development. Prioritizing these essentials ensures both you and your little one thrive.
The benefits of a balanced diet extend far beyond pregnancy. They lay the foundation for lifelong health for both mom and child. Regular prenatal care and thoughtful meal planning are key to achieving these goals.
As you prepare for the postnatal phase, continue focusing on nutrient-rich foods. This supports recovery and provides the energy needed for breastfeeding. Start planning your meals today to make the most of this special time.