Pregnancy loss is more common than many realize, affecting 10-20% of known pregnancies. Most occur in the first trimester, often due to factors beyond anyone’s control. While it can be emotionally challenging, understanding the causes helps dispel myths and offers reassurance.
Chromosomal abnormalities account for half of early losses, according to medical experts. Other factors include hormonal imbalances or health conditions. Contrary to popular belief, everyday stress or moderate exercise does not trigger pregnancy loss.
This article explores eight key insights, from risk factors to emotional support. Knowledge empowers, whether you’re planning a family or navigating early pregnancy.
Key Takeaways
- 1 in 5 pregnancies may end in loss, often in the first 12 weeks.
- Chromosomal issues cause 50% of early pregnancy losses.
- Most miscarriages cannot be prevented.
- Stress and exercise are not proven causes.
- Medical guidance clarifies non-causal factors.
Understanding Miscarriage: An Overview
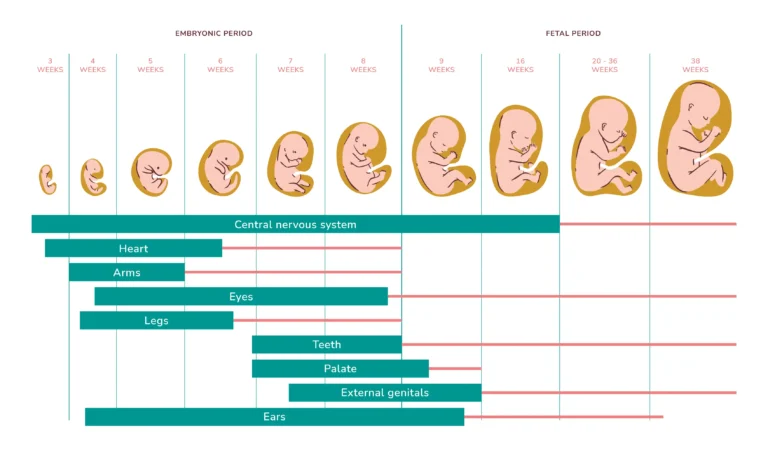
Many early pregnancies end before a woman even realizes she’s expecting. Medically, pregnancy loss before 20 weeks is called a miscarriage, while later losses are termed stillbirths. Most occur in the first trimester, often due to chromosomal issues.
Chemical pregnancies—very early losses—account for about 30% of cases. The body naturally stops pregnancies that aren’t viable, often passing tissue with bleeding. This doesn’t mean future pregnancies will face the same outcome.
Doctors use ultrasounds or hCG blood tests to confirm a loss. Contrary to myths, everyday activities like exercise or stress rarely cause it. The American College of Obstetricians (ACOG) notes: “Most losses are random, not preventable.”
Recovery varies: physical healing may take weeks, while emotional healing can take longer. Recurrent loss (3+ times) affects 1% of couples and warrants specialist care.
What Causes Miscarriage?
Several factors contribute to early pregnancy loss, from genetics to lifestyle. While each case is unique, research identifies common triggers. Below are the primary categories.
Chromosomal Abnormalities
50% of first-trimester losses stem from chromosomal errors. These occur when embryos develop extra or missing chromosomes. The body often naturally ends non-viable pregnancies.
Age impacts egg quality, raising risks. For example, women over 35 face higher odds of such errors. This doesn’t reflect parental health—it’s a random biological event.
Health Conditions and Infections
Chronic illnesses like diabetes or thyroid disease can affect pregnancy. Autoimmune disorders (e.g., lupus) may trigger immune responses against the embryo.
Infections also pose risks:
- TORCH diseases (e.g., CMV, toxoplasmosis).
- Listeria from unpasteurized foods.
- STIs like syphilis.
Uterine or cervix issues—such as an incompetent cervix—account for 15% of recurrent losses.
Lifestyle and Environmental Factors
Smoking increases risks by 40%, while heavy alcohol use disrupts fetal development. Toxins like lead or pesticides are also linked to higher rates.
Debunked myths: Moderate caffeine (under 200mg/day) and exercise are safe. Stress alone rarely causes loss.
| Factor | Risk Increase | Notes |
|---|---|---|
| Smoking | 40% | Quitting reduces odds |
| Uterine abnormalities | 15% | Often treatable |
| Untreated diabetes | 2x | Managed cases lower risk |
While some factors are controllable, many aren’t. Focus on manageable changes, like prenatal care and avoiding toxins.
Symptoms and Signs of Miscarriage
Physical and emotional symptoms vary widely, but understanding them brings clarity. While some cases involve noticeable changes, others may show no outward signs. Early awareness helps in managing expectations and seeking care when needed.
Common Physical Symptoms
Bleeding is the most frequent sign, ranging from light spotting to heavy flow. About 90% of cases involve vaginal bleeding, often accompanied by clots or tissue. Cramping may feel like period pain or intensify into severe discomfort.
Other warning signs include:
- Fever or chills (indicating infection risk).
- Foul-smelling discharge.
- Sudden loss of pregnancy symptoms (e.g., breast tenderness).
In missed cases, an ultrasound may detect no heartbeat despite no bleeding. Always consult a doctor for unusual pain or prolonged symptoms.
Emotional and Psychological Signs
Grief, guilt, or shock are normal reactions. Emotional recovery varies—some heal in weeks, while others need months. Support groups or counseling can provide solace.
When to seek help: Persistent heavy bleeding, dizziness, or fever require urgent care. For emotional distress, therapists specializing in pregnancy loss offer tailored support.
Risk Factors for Miscarriage
Certain health and lifestyle factors can influence pregnancy outcomes. While some risks are unavoidable, others can be managed with medical guidance. Recognizing these factors helps in planning and reducing unnecessary stress.
Age and Recurrence Risks
Age significantly impacts pregnancy viability. Women over 40 face a 25% risk—double that of younger individuals. After one loss, recurrence odds rise to 25%, but most go on to have healthy pregnancies.
Recurrent loss (2+ times) affects 1% of couples and often signals underlying health conditions. Genetic testing or uterine evaluations may uncover causes like PCOS or low progesterone.
Medical and Genetic Influences
Chronic disorders like diabetes or thyroid disease heighten risks if unmanaged. Uterine abnormalities (e.g., fibroids) account for 15% of recurrent cases. Male factors, such as sperm DNA fragmentation, also contribute.
Key modifiable risks include:
- Obesity (20% higher risk).
- Smoking or toxin exposure.
- Untreated infections (e.g., STIs).
| Factor | Risk Increase | Actionable? |
|---|---|---|
| Age 40+ | 25% | No |
| Obesity | 20% | Yes |
| Uterine issues | 15% | Often treatable |
Preconception counseling helps address modifiable risks. For IVF pregnancies, close monitoring improves outcomes. Knowledge empowers proactive care—whether managing conditions or seeking specialist support.
Types of Miscarriage
Not all pregnancy losses present the same way—understanding the differences helps in seeking proper care. Doctors categorize them based on symptoms, progression, and diagnostic findings. Knowing what to expect can ease anxiety and guide next steps.
Threatened vs. Complete Loss
A threatened miscarriage involves vaginal bleeding or cramping, but the pregnancy continues. About 20% of cases resolve without further issues. Key signs include light bleeding and mild pain, often monitored via ultrasound.
In a complete loss, all pregnancy tissue passes naturally, usually within two weeks. Bleeding may be heavier, resembling a period. Doctors confirm it with an ultrasound showing an empty uterus.
Missed and Recurrent Losses
A missed loss occurs when the embryo stops developing, but the body doesn’t expel tissue. No bleeding or pain may occur, making an ultrasound critical for diagnosis.
Recurrent loss (2+ times) affects 2% of pregnancies. Causes include:
- Uterine abnormalities (e.g., septate uterus).
- Asherman’s syndrome (scarring).
- Chromosomal errors (testing identifies these).
Despite challenges, 65% of couples later have successful pregnancies. Specialists may recommend surgery or hormonal therapy to address underlying issues.
Treatment and Recovery After Miscarriage
Recovering from pregnancy loss involves both medical care and emotional healing. Treatment options depend on individual circumstances, from natural passing to surgical intervention. Knowing what to expect can ease the journey toward recovery.
Medical and Surgical Options
Doctors may recommend:
- Expectant management: Letting tissue pass naturally (4–6 weeks).
- Medication: Misoprostol helps the uterus expel tissue faster.
- Dilation curettage (D&C): A 95% effective surgical procedure to remove remaining tissue.
Rh factor matters—if blood tests show you’re Rh-negative, a shot prevents future complications. Post-procedure, watch for fever or heavy bleeding (>2 pads/hour).
| Option | Timeframe | Considerations |
|---|---|---|
| Expectant | 4–6 weeks | No surgery, but unpredictable |
| Medication | 1–2 days | Cramping common |
| Dilation curettage | 1 day | Quick recovery, minimal pain |
Physical and Emotional Recovery
Your period typically returns in 4–6 weeks. Hormonal shifts may cause mood swings—this is normal. Partners grieve differently; open communication is key.
Support groups (like March of Dimes) offer solace. Memorialization ideas, such as planting a tree, can provide closure. Seek help if grief persists beyond 2 months.
Returning to intimacy: Wait until bleeding stops and you feel emotionally ready. Doctors often recommend 2 weeks post-D&C.
Pregnancy After Miscarriage: What to Know
Planning another pregnancy after loss can feel overwhelming, but understanding key steps brings confidence. 65% of couples conceive within six months with proper care. Focus on physical readiness and emotional healing to build a strong foundation.
Preparing for a Healthy Pregnancy
Doctors often recommend waiting 1–3 menstrual cycles before trying again. This allows hormone levels to stabilize. Preconception tests improve outcomes:
- Thyroid panels and glucose checks
- Folic acid levels (600mcg daily reduces risks)
- Infection screenings for STIs or TORCH diseases
Lifestyle adjustments matter. Quit smoking, limit caffeine, and manage stress through yoga or therapy. Partners should join appointments—shared understanding strengthens support.
When to Seek Specialist Help
Consult a fertility specialist after two losses or if you’re over 35. Recurrent loss workups may include:
- Genetic carrier screening
- Hysteroscopy for uterine abnormalities
- Sperm DNA fragmentation tests
MFM specialists (Maternal-Fetal Medicine) manage high-risk cases. REI consultations cut recurrence odds by 50%. Insurance often covers these visits—check your plan’s details.
Anxiety is normal. Therapists specializing in pregnancy loss offer coping strategies. Success rates remain high with tailored care.
Conclusion
Healing after pregnancy loss takes time, and every journey is unique. While grief is natural, 65% of couples go on to have healthy pregnancies with proper care and support.
Lean on loved ones or professional counselors—you’re not alone. Memorials, like planting a tree, can honor your experience. Follow-up visits ensure physical health, while therapy aids emotional recovery.
Remember: pregnancy loss is rarely preventable. Focus on manageable steps—prenatal vitamins, stress reduction, and open communication with your doctor. For immediate help, contact the Pregnancy Loss Support Hotline (1-800-221-7437).